 Back Up
Back Up Back Up
Back UpLook at the Immediate Clinical History
Take a Personal History
Platelet
Count
Two major techniques are used for automated platelet measurements. They use
size thresholds to distinguish between platelets, leucoytes and erythrocytes.
Normal number 150 to 400x109/L.
The machines are accurate and reliable down to 10-30x109/L but are subject
to specimen error:
Genuinely low levels are due to
Platelet Aggregation
The addition of an agonist (thrombin, ADP, adrenaline, collagen, ristocetin or
arachnidonic acid) to platelet rich plasma normally exhibits a biphasic response of
reversible aggregation due to the agonist followed by irreversible aggregation due to the
disintegration of the platelets.
Heparin induced platelet aggregation
Used in the diagnosis of heparin-associated thrombocytopaenia.
Hess Test
In vivo assessment of collagen matrix, vascular endothelium and platelet adhesion and
aggregation
A syphgomomanometer is inflated to between the systolic and the diastolic pressures
for 10 minutes. Normal less than 15 petechiae would occur in a 5cm diameter
circle.
Quick labeled the test prothrombin time when he devised it in 1935 as he believed
it was a simple, accurate, and sensitive measure of prothrombin. He was wrong.
The specimen should be a 3.8% trisodium citrate anticoagulant in a 9:1 ratio with the
blood, which is centrifuged to produce platelet poor plasma. A complete
thromboplastin (typically from rabbit brain) is then added with calcium. The time to
fibrin strand formation is then measured automatically by:
Many variables affect the prothrombin time
A Normal INR is between 0.9 and 1.2
Prolonged = Deficiency of factor I, II, V, VII or X. The test is most sensitive to decreases in factor VII which is one of the vitamin K dependant factors.
- Coumarin anticoagulation therapy
- Vitamin K deficiency
- Severe Liver disease
- Massive blood transfusions
- Disseminated intravascular coagulation
- High dose heparin therapy
This test derives its name from the use of a partial thromboplastin, or "cephalin" which is a phospholipid component that is added to a specimen that has been "activated" by exposure to a negatively charged substance (kaolin, celite or ellagic acid).
Normally 25 to 35 seconds
Prolonged = A decrease to less than 30% activity of all the coagulation factors
Errors in specimen collection will also affect the result
Normal plasma and the patient's plasma are compared in their ability to correct the INR or aPTT of plasma from an individual severely deficient in the factor of interest.
By convention normal plasma is said to have 100% or 1 unit per ml activity. If a 1:10 dilution of a specimen has the correcting power of a 1:100 dilution of normal plasma, the specimen has 10% or 0.1 unit per ml activity.
The mixing study
The patient's serum is mixed with normal serum and the aPTT of this mixture is measured.
A 50:50 mixture will correct a factor deficiency (only 30% activity is needed for a
normal aPTT). In the presence
of an inhibitor a 50:50 mix will not correct the abnormal coagulation test.
Factor VIII inhibitors
Lupus Anticoagulant
Thrombin is added to plasma and the time taken to form a clot is recorded Normal is less than 15 seconds
Prolonged due to inhibition of thrombin
- Heparin
- Fibrin degradation products
- Lupus anticoagulant
Prolonged due to abnormal fibrinogen
Reptilase is added to plasma and the time taken to form a clot is recorded. Normal is less than 14-19 seconds
A sphygmomanometer on the upper arm is inflated to 40mmHg. A skin incision 5mm long and 1mm deep is made on the extensor surface of the forearm, using a spring loaded template device.. The wound avoids scar tissue and superficial vessels, and must be done within 60 seconds of inflating the sphygmomanometer. Filter paper is used to blot the edges of the wound at 30 second intervals until the bleeding stops. Normal is two to nine minutes
According to Rodgers & Levin:
[A critical reappraisal of the bleeding time. Sem Thromb Haemost 1990: 16: pp1-19]
Conventional theory alleges that a prolonged bleeding time is due to
Fresh whole blood is added to a tube containing negatively charged particles and timed for the formation of a clot.
The type of negatively charged particle affects the "normal" length of ACT
Celite = Diatomaceous Earth: normal is 100-170 seconds
Kaolin: normal is 90-150 seconds
Glass particles: normal 110-190 seconds
None: normal 190-300 seconds
Type of machine affects normal and therapeutic values
Hemochron
A warmed test tube is rotated inside the machine. As the blood clots, it displaces the magnet within the test tube. The clotting time is determined when the magnet has displaced enough to activate a proximity switch
Medtronic HemoTec
A mechanical plunger is dipped in and out of a kaolin activated blood sample. The machine optically senses the time it takes the plunger to move through the specimen. Clotting is defined by the "drop time" threshold for the plunger
The machines do not correlate with one another but in general the times for the Hemochron are 30% greater than the Medtronic HemoTec
Specimen quality affects the values
Daily calibration checks are imperative
Clinical use of the ACT in assessing adequacy of heparinisation
Prolonged times may be due to
- Heparin effect
- Hypothermia
- Platelet dysfunction
- Haemodilution
- Cardioplegic solutions
- Hypofibrinogenaemia
- Factor deficiencies
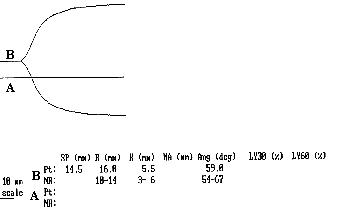
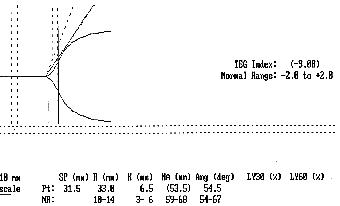
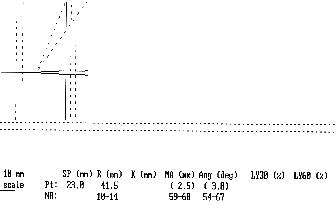
A Sample of celite activated whole blood (0.4ml) is placed into a pre warmed cuvette. A pin suspended from a torsion wire is then lowered into the cuvette. The cuvette is rotated backward and forwards in a small arc. As the fibrin strands interact with the activated platelets on the surface of the pin, the rotational movement of the cuvette is transmitted to the pin. The stronger the clot the more the pin moves. The Haemoscope is connected to a computer and the coagulation profile is then displayed on the screen as an outline of a Thromboelastograph
There are 6 parameters of importance in a TEG tracing
R value = This is the period of time from initiation of the test to the initial fibrin formation and pin movement
k value = This is the measure of time from the beginning of clot formation until the amplitude of the TEG reaches 20mm.
alpha angle = This is the angle between the line in the middle of the TEG tracing and the line tangential to the developing "body" of the TEG
Maximal Amplitude = This is the greatest amplitude of the TEG tracing
Amplitude at 60 minutes = This is the amplitude of the TEG tracing 60 minutes after the Maximal Amplitude is recorded.
Clot Lysis Index = The amplitude at 60 minutes expressed as a percentage of the maximal amplitude.
Normal Thromboelastogram
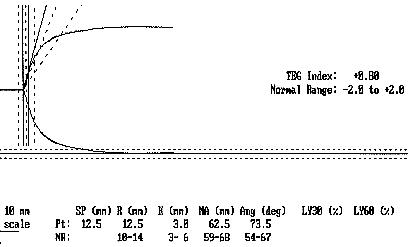
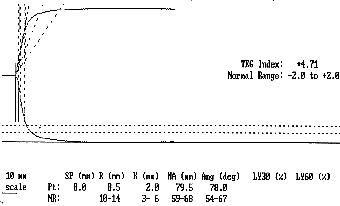
Alterations of the normal TEG pattern can give information about
The coagulation factor activation - R value
The coagulation factor amplification - k value and alpha angle
The platelet aggregation - Maximal Amplitude
Fibrinolysis - Amplitude 60 minutes after Maximum
Platelet adhesion to the collagen matrix is not assessed
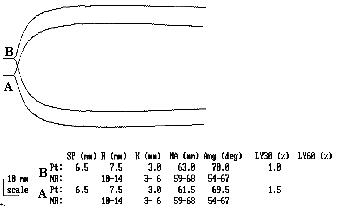
Example 1
Example 2
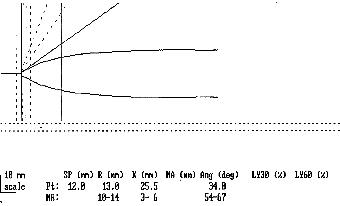
Example 3
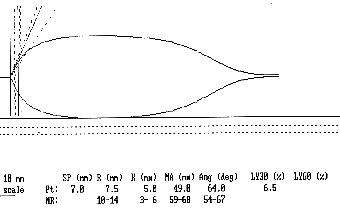
Example 4
Example 5
Example 6
Example 7
Example 8
Peri-operative & ICU Anticoagulation
Bibliography
Web Page Author: hopley@anaesthetist.com